Scoliosis treatment
Primary prevention of spinal curvature: pathological posture, scoliosis, juvenile kyphosis, Scheermann-Mau disease.
Reasons, classification of curvature of the spine.
There are many versions of the reason for the occurrence of scoliotic deformity and there are more and more of them every day, respectively, and there are more and more proposed treatment methods, but, unfortunately, some of them cannot be criticized, sometimes they are effective, but also hazardous to health.
Scoliosis (scoliosis; Greek skoliosis curvature) is a disease of the musculoskeletal system, characterized by a curvature of the spine in the frontal (lateral) plane with a turn of the vertebrae around its axis, leading to impaired chest function, as well as cosmetic defects.

The spine, when viewed from behind, should be straight. In some, however, it takes an S-shape (scoliosis). In mild cases, this does not lead to any complications. With significant curvature of the spine, when it rotates around its axis, sometimes pain occurs and its ability to function normally decreases. From the point of view of biomechanics, the process of formation of scoliotic deformity–is the result of the interaction of factors that violate the vertical position of the spine and adaptive reaction aimed at maintaining a vertical posture. Therefore, treatment of scoliosis in such cases is mandatory.
The term «scoliosis» refers to lateral curvature of the spine. Moreover, this term is used both in relation to the functional bends of the spine in the frontal plane («functional scoliosis», «scoliotic posture», «antalgic scoliosis»), and in relation to progressive a disease leading to complex, sometimes severe, deformity of the spine («scoliotic disease», «structural scoliosis»).
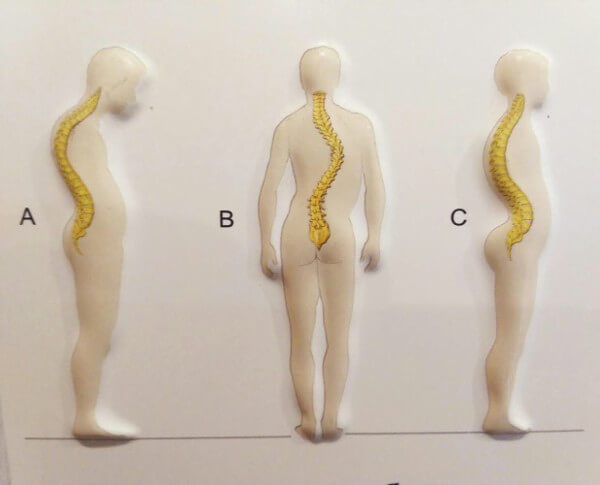
Scoliotic disease, or scoliosis , in contrast to the functional curvature of the spine in the frontal plane, is characterized by wedge-shaped and torsion deformity of the vertebrae progressing during growth, as well as deformation of the chest and pelvis.
Structural scoliosis develops with some metabolic diseases leading to functional inferiority of connective tissue structures– Marfan syndrome, Ehlers-Danlos syndrome, homocystinuria, pick it up. With these diseases, scoliotic deformation acts as one of the symptoms, and not the most important one.
Static scoliosis is usually called structural scoliosis, the primary cause of which is the presence of a static factor–of asymmetric load on the spine due to congenital or acquired asymmetry of the body (for example, asymmetry of the length of the lower extremities, pathology of the hip joint or congenital torticollis.). With static scoliosis, the rate of progression and the severity of deformation depend on the ratio of the severity of the static factor and the factor of functional failure of the structures, those who hold the vertical position of the spine. With a good functional state of the musculo-ligamentous apparatus and intervertebral discs, curvature of the spine can remain functional in nature for a long time or not lead to the development of progressive scoliosis. As long as the pulpous nucleus of the intervertebral disc maintains a central position, the pressure of the body weight transmitted to the disc is distributed evenly over the entire area of the supporting platform of the underlying vertebra, without causing progressive wedge-torsion deformation. If, in the presence of a slightly pronounced static factor, the compensatory mechanisms are weak or there is a functional inferiority of the connective tissue structures, the scoliotic factor forms and causes the progression of deformation. With functional muscle failure, most of the load to maintain a vertical posture is transferred to the ligaments. A sufficient degree of ligament tension is achieved due to a significant increase in the angle of curvature of the spine, leading to an increase in the load on the intervertebral discs, persistent lateral displacement of the pulp nucleus, and thus the formation of a scoliotic factor. Static compensation of gross asymmetry of the body can be achieved due to significant curvature of the spine. At the same time, the intervertebral discs are subjected to a large asymmetric load, which leads to the formation of a scoliotic factor even in the absence of dysplastic changes, muscle weakness, and constitutional weakness of connective tissue structures.
With scoliotic disease, allocated in a separate nosological form, curvature of the spine – is the main symptom. The term «scoliotic disease» combines congenital, dysplastic and idiopathic scoliosis (i.e., scoliosis of unknown origin). Congenital scoliosis is caused by gross skeletal malformations, such as additional lateral cuneiform vertebrae of the vertebra. With congenital scoliosis, the shape of the curvature is directly dependent on the location and nature of the anomalies.
The reason for the development of dysplastic scoliosis – dysplasia of the intervertebral disc, expressed in the eccentric location of the pulpous nucleus. With dysplastic scoliosis, bone abnormalities such as failure of the vertebral arches are often detected, violation of the tropism of the articular processes, S – I lumbarization, L – V sacralization, indicating the presence of «dysplastic syndrome». With the so-called idiopathic scoliosis by modern means of examination, it is not possible to identify the immediate causes of the development of curvature of the spine.
In adolescence, sometimes there is another, more dangerous form of curvature of the spine, the exact cause of which is unknown. Here we are talking about Scheuermann-Mau disease. The disease occurs due to uneven areas of the bodies of the affected thoracic, less often upper lumbar vertebrae. The affected vertebrae lag behind in growth in height, kyphosis is formed here, later– thinning of the intervertebral discs. Deformation in this case is very severe, pain and a feeling of «stiffness» in the spine, rapid fatigue are felt. For the adolescents in question, the curvature also entails significant psychological trauma. Mechanogenesis of the development of deformity in Scheuermann-Mau disease is as follows:
- The primary pathological kyphotic deformity in the thoracic spine leads to a shift in the center of gravity of the trunk to the front. In response, to compensate for this pathological condition, the entire body is tilted back due to a turn of the pelvis in the hip joints, since this compensation mechanism is the most effective.
- The newly emerged biomechanical situation leads to a change in the loads in the lumbar spine, which, being less rigid than the thoracic spine, continues to bend under the influence of increased bending loads due to an increase in the shoulder, which leads to a gradual increase in lumbar lordosis. The continued increase in lordosis inevitably leads to the loss of the vertical position of the trunk. To prevent this situation, as the lumbar lordosis intensifies, the pelvis gradually returns to its normal position.
- The created new pathological biomechanical situation of system equilibrium does not exclude further progression of both breast kyphosis, and lumbar lordosis. The torso muscles involved in the compensation process fix the position of the pelvis and thereby turn off the initial compensation mechanism. Now, the continuing increase in thoracic kyphosis can only be compensated by flexion in the knee and hip joints, as the physiological possibilities of over-extension of the lumbar motor segments are also exhausted. Flexion in the knee and hip joints most clearly affects the change in the spatial position of the thoracic spine, which is manifested in a change in the position of the chord of its arc.
- A typical patient posture is formed, which allows you to keep the torso in an upright position, but does not prevent the slow progression of breast kyphosis, which becomes rigid with age and with the completion of the restructuring of the vertebral bodies.
- The resulting inclination in the true joints of the lumbar spine leads to the appearance of a pain syndrome, and the growing deformation– to the appearance of neurological symptoms of a conflict between the spinal cord and the spinal canal.
Treatment of curvature of the spine and treatment of scoliosis.
Treatment of scoliosis consists of three interrelated links: mobilization of the curved spine, correction of deformation and stabilization of the spine in the position of the achieved correction. Manual methods of manual therapy are very effective for correcting spinal deformity. The maintenance of the achieved correction with their help can only be promoted indirectly, through the formation of a new static-dynamic stereotype adapted to the changes introduced into the shape of the spine. The change in the static-dynamic stereotype is carried out by deliberately influencing the links of the musculoskeletal system above and below the main curvature and regulating the tone ratios of the conjugated muscle groups involved in posture formation. However, the main and most difficult task, the solution of which determines the success of treatment of scoliosis as a whole, is not mobilization and correction of curvature, but stabilization of the spine in a corrected position. Correction of the deformity, not supported by measures to ensure stabilization of the spine, is ineffective.

Conservative methods of treatment of scoliosis cannot directly affect the structural changes of the spine. Therefore, attempts to mechanically «straighten» the curvature of the spine caused by the structural reconstruction of the vertebrae and intervertebral discs are pointless. The essence of conservative treatment is to correct spinal curvature by reducing the functional component of the curvature and stabilizing the achieved correction by improving the functional state of the musculo-ligamentous apparatus or using corsetry.

