Quite often, joint pain mimics the damage to the tissues around the joint - this is damage to the tendons (tendinitis), muscles (myotendinitis), fascia (fasciitis), tendon vagina (tendovaginitis). This is a group of diseases that can be closely related to joint damage, or occur independently. Soft tissue surrounding any joint may be affected.
Periarthritis of the hip joint (trochanteritis) - it is based on degenerative changes and secondary inflammatory changes in the tendons of the middle and small gluteal muscles. The main causes are overload, hypothermia, low mobility and obesity. Trochanteritis is manifested by pain in one of the hip joints, in the area of the buttocks and one of the swivels. The pain is exacerbated by exercise. The pain can be moderate, and it can be very intense and resemble acute coxitis. It is possible to develop chronic tendobursitis with constant alternation of exacerbations and improvements.
Periarthritis of the knee - occurs as a result of everyday, professional and sports microtrauma, due to constant flexion, extension, external rotation, leading to the appearance of degenerative changes and secondary inflammatory reaction. The main manifestation is pain when pressed on the inner surface of the knee joint and at the moment of flexion of the joint when walking.
Periarthritis of the foot (spurs of calcaneus)- often occurs with lesions of the attachment points of the Achilles tendon, sinews of the plantar muscles to the heel bone. The lesions can have both degenerative and inflammatory origin. Degenerative changes occur as a result of overload and microtraumas (running, running), when at too high a tension of these tendons, the fibrils burst with the further development of their degeneration. Spurs and plantar fasciae can also be manifestations of other inflammatory conditions in the body such as ankylosing spondylitis, reactive arthritis, gout, psoriasis. In this case, it is important to identify and treat the underlying disease. The pathological process ends with the formation of bone growths in the area of the lesion, ie spurs. For heel spurs there is a pain in the heel that occurs when pressing on the heel. In the area of the Achilles tendon is visible round, painful formation (Achillobursitis), and the tendon itself is thickened and painful when pressed (Achilles). The radiograph shows spurs on the posterior or plantar surface of the calcaneus.
The periarthritis of the elbow joint includes external epicondylitis (tennis elbow) and internal epicondylitis (epitrochleitis) and olecranalgia. Tennis player's elbow - the tendons of the extensor tendon and toes are affected, long forearm supporter, characterized by pain in the area of the outer surface of the elbow and painful restriction of movement, pain is given on the outer edge of the shoulder and down to the middle of the forearm. Pain occurs when extending and supination of the forearm. The pain is also exacerbated by the clenching of the wrist into the fist and its flexion at the same time. Strength in the wrist is reduced. Diseases are associated with the occupational and athletic trauma of people who often repeat stereotyped movements in the elbow joint.
Internal epicondylitis of the shoulder is caused by degenerative changes of the tendons of the flexors of the tendon, fingers and one of the heads of the round pronator of the forearm. Occurs at typists, seamstresses. Pain occurs when pronation and flexion of the forearm and extends along the inner edge of the forearm.
Olekranalgia - it is characterized by constant pain in the area of the elbow, which occurs as a result of degenerative changes in the area of attachment of the tendons of the three-headed muscle to the elbow. The disease usually begins after the injury.
Periarthritis of the radial - wrist joint (stiloiditis) - the tendon of the long supinator of the forearm is damaged in the place of its attachment to the subulate process. Dressmakers are more likely to suffer from occupational micro-traumatization. The main symptom is pain in the area of the subulate process of the radial bone, exacerbated by supination of the forearm. A slight swelling is noted in this area.
Lesions of the tendons of the rotator cuff of the shoulder, shoulder scapular periarthritis, impingement syndrome.
The muscles of the rotator cuff of the shoulder joint include subacute, supraspin, subclavian and small round muscles. These muscles and their tendons are also called the second humerus, the first represented by bone structures: the humerus and shoulder blade (actually the humerus). The tendons of the above mentioned muscles can be damaged as a result of degenerative changes (age, overload, possible infections) and trauma. Similar injuries can be caused by spondylosis of the cervical spine, lesions of the shoulder plexus, be a consequence, heart attack, and congenital anomalies of the development of the upper shoulder girdle.
Usually, as a result of micro-injuries, tendons are inflamed at the site of attachment to the bone and serous bags (bursitis) nearby are inflamed.
How these conditions manifest themselves: A characteristic symptom of impingement syndrome is pain and movement limitation in the shoulder joint. The pain is exacerbated when lifting your arms up and trying to lay your hand behind your back and head. Also, the pain is exacerbated when pressed in the area of the front upper part of the shoulder at the place of attachment of the tendons of the rotators. Passive movements in the shoulder may not cause pain.
If left untreated, it goes into the least favorable form. It is also called "blocked or frozen shoulder". It is based on fibrotic changes in the capsule of the shoulder joint, which lead to the fact that movements in the shoulder joint are impossible. Movements occur only due to the scapular - sternal connection. This condition requires surgery, unlike the initial manifestations of shoulder blade periarthritis.
First of all, the treatment of the affected joint and its corresponding fixation are included in medical measures. Non-steroidal anti-inflammatory drugs as well as topical steroid injections are prescribed for pain relief and inflammation.
In addition to the above-mentioned remedies, the clinic "Health Practice" is widely used in physiotherapy, which have anti-inflammatory and protective effects. Their use significantly enhances the anti-inflammatory effects of drugs and improves metabolism and nutrition in the degenerately damaged areas of the tendons of the rotator cuff of the shoulder.
After the joint pain decreases, the volume of movements increases, the next stage of treatment begins, this is the effect on the cause. If it is spondylitis (osteochondrosis) of the cervical spine, then its treatment is carried out in order to prevent relapses. Appropriate physiotherapy procedures and therapeutic gymnastics are prescribed under the close supervision of doctors. If the cause is in the degenerative conditions of the joint and tendons (deforming osteoarthritis, tendinitis), then the corresponding physiotherapy and drug treatment of the latter is carried out with the subsequent training of the gymnast. Of particular importance is prevention. Conversation with the patient about the importance of treatment at the initial stage of the disease and informing him about the possible complications and features of their subsequent treatment.
Myotendinitis
They usually occur in people with heavy physical labor, most commonly affected by the extensors of the tassels and feet. Characteristic pain in movements involving the affected tendon and muscle. For example, when lesions of the radial extensors tendon pain, redness and swelling are localized in the area of the posterior tendon, in the case of the defeat of the muscles of the thumb - in the area of the pylid process, the Achilles tendon - above the heel. Pain usually occurs during active movements, passive movements are not painful. These conditions are difficult to treat and have a tendency to relapse.
Tendovaginitis
Inflammation or degenerative changes in the middle part of the tendon, these are the places that pass through the tendon sheath (narrow ducts). In this condition there is difficulty in sliding the tendon through the narrow canal for a number of reasons: thickening of the tendon, narrowing of the canal, scar changes of the canal. The site of the lesion determines the symptoms and accordingly the proper name of tendovaginitis.
De-Kerwen's disease: tendon vaginitis of the muscle that takes away the thumb. Occurs as a result of thumb overload. It is manifested by pain and swelling in the area of the subulate process, which is exacerbated by flexion and abduction of the thumb. The force in the finger decreases.
Elbow styloiditis: also manifested by pain in the area of the subulate process of the elbow bone, the pain is exacerbated by the removal of the tendon towards the radial bone. The pain also gives 4 and 5 fingers.
Carpal tunnel syndrome: flexor tendon tendonitis or wrist stenosis of the transverse palmar ligament. A pathological process occurs in the canal as a result of an inflammation, injury, or tumor that leads to a contraction of the median nerve that runs in that canal. This syndrome is manifested by severe pain in the 1, 2, 3 fingers of the affected tendon, which is aggravated at night. Characteristic swelling of the fingers and tendons, increased sweating of the area, possible atrophy of the muscles, and in severe cases the appearance of trophic ulcers at the tips of the fingers.
Guillon canal syndrome: the wrist is also affected, only a pathological process occurs in the Guillon canal, located on the side of the elbow edge of the ligament. The elbow nerve and the ulnar artery pass through this canal. The compression of these structures causes pain, mainly at night, sensation of constipation and trophic disorders in the 4 and 5 fingers of the tendon.
Knott's disease: occurs as a result of the development of tendovaginitis of the superficial flexors of the fingers and stenosing ligamentitis of the annular ligaments of the fingers, as a consequence of occupational microtrauma. Pain manifested in the base of the 1, 2 and 4 fingers of the tendon when moving and pressing on the specified area. Pain can be given to the wrist and forearm. When bending and extending, there is a painful obstruction, which overcomes the click. At this point, the deformed tendon passes under the ligament.
Torsal canal syndrome: develops with tendon and vaginitis of the posterior tibial muscle and stenosing ligamentitis of the posterior ligament canal of the inner surface of the ankle and foot. The syndrome occurs as a result of contraction of the posterior tibial nerve. Muscle pain and the feeling of crawling on the inner surface of the foot and fingers occur. Sensitivity disturbance on the dorsal surface of the foot is noted.
Treatment of tendovaginitis and periarthritis is based on similar principles. This is the tranquility of the affected area with the use of tires and longnet. Use of analgesics and anti-inflammatory drugs. An important factor in achieving a tangible therapeutic effect is the use of electrotherapy, diathermy, iontophoresis with hydrocortisone. After the anti-inflammatory effect is achieved, it is necessary to begin therapeutic gymnastics (passive movements) in order to maintain normal function of the muscles and tendons in the affected area. All these types of assistance are provided at the Medical Practice under constant medical supervision.
Bursitis and tendurs
This inflammation in serous bags usually accompanies other lesions of the joints and around the joint tissues. At the same time in serous bag accumulate effusion, with time in this place deposited calcium salts. Bursites can be superficial (elbow, prepatellar) and deep (subtalar). With superficial bursitis pain is noted, and subcutaneous, elastic, soft formation.
- With purulent bursitis, the pain can be severe. The skin above it is red. Sometimes you can feel calcinates under your skin.
- In deep bursitis, pain and restriction of movements in the adjacent tendons and joints, as well as signs of deposition of calcium salts in the locations of the bags and tendons seen on radiographs are noted.
- The humeral bursitis arises under the sub-deltoid muscle; the elbow is located superficially between the skin and the ulnar process;
- The swivel of bursitis occurs with trochanteritis of the hip joint at the place of attachment of the gluteal muscles;
- The gluteal bursitis develops between the gluteal tubercle and the large gluteal muscle;
- Pre-patellar bursitis is located between the knee and the skin;
- The popliteal bursitis (Baker's cyst) is located in the popliteal serous pouch and connects to the cavity of the knee. Therefore, most often, Baker's cyst is the result of problems in the knee joint.
Treatment is also associated with a reduced load on the affected area. If the disease is related to occupational activity, it is recommended to change the type of activity. Medication and physiotherapy measures are similar to those prescribed for tendovaginitis and periarthritis.
Fasciitis and aponeurosis
This is called fascia inflammation and aponeurosis. Most often they develop as a result of injuries (physical, mechanical and thermal), as well as in some infectious, metabolic, endocrine and allergic diseases. At the beginning of the disease, an effusion is formed, then a seal of this effusion, and at the final stage of the formation of scar changes. Close contact between the muscles and the fascia results in fibromyositis. The most commonly affected are wide fascia of the thigh, lumbar and cervical fascia, palmar and plantar aponeurosis.
Fasciitis and aponeurositis present with pain and stiffness in the area of the affected fascia, and dense painful nodules appear, which may disappear or enlarge. Typical muscle atrophy. Aponeurosis may result in the formation of contractions of the affected aponeurosis with a sharp limitation of motility in the corresponding area of the aponeurosis. However, the pain may not bother.
When the broad fascia of the thigh is affected, pain and nodular seals are noted on the lateral surface of the thigh. Movements in the thigh may click. Lumbar fasciitis (lumbar fibromyositis) is characterized by painful nodules in the lumbar region, which often accompanies chronic low back pain.
Dupuytren's contracture: chronic inflammation of the palmar aponeurosis with progressive fibro-scar changes. The tendons 4 and 5, and sometimes 3 fingers, are involved in the process. A steady bending contracture in the metacarpophalangeal and proximal interphalangeal joints is gradually formed. The palms of the palms of the 4 and 5 fingers appear on the palm of the palm, and the tendons are tightened and shortened, which look like tightly-wired harnesses. These fingers are in a state of incomplete, and then complete flexion. Usually there is no pain.
Lederhosis contracture: it is based on a process similar to Dupuytren's contracture, only the lesions of plantar aponeurosis. In the last stage of the disease, the toes are in a constant state of flexion.
Treatment of fasciitis and aponeurositis: first of all, it provides peace of the affected area. Allergic and other factors that could cause the disease should be avoided. Physiotherapy and physiotherapy are of key importance in treatment. The most effective are diathermy, electrotherapy, massage and infiltration of the affected area with hydrocortisone. This helps to reduce inflammation in the affected area, improve blood supply and reduce pain. Therapeutic exercise prevents the formation of irreversible scar changes in the aponeurosis, that is, the appearance of contracture. Medical Center "Health Practice" has wide possibilities for effective treatment and prevention of irreversible changes in fascia, aponeurosis and tendons. Treatment of aponeurosites makes it possible to avoid the development of late stages and, accordingly, surgical interventions at the site of contracture formation.
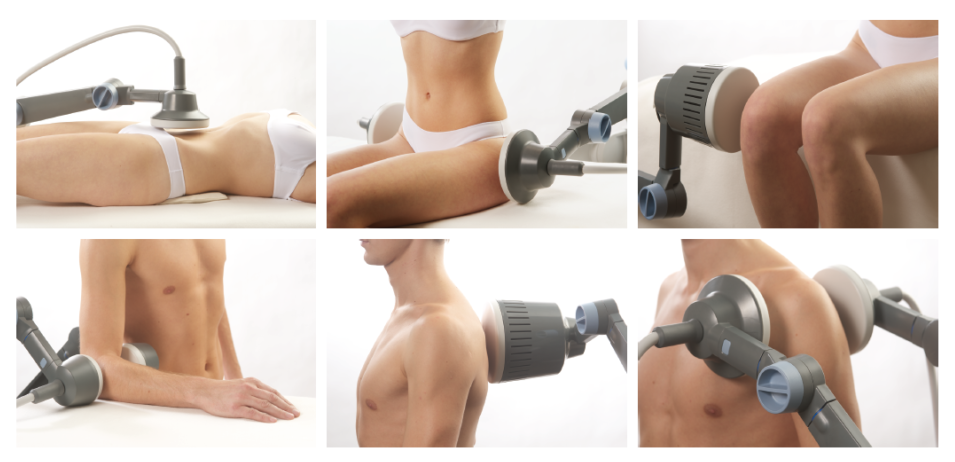
General principles of treatment of soft disease around the joint tissues in the clinic "Health Practice"
The peculiarity of treatment in the clinic is a combination of the latest physiotherapy effects on the body or the affected area of the body. It is the combination of effects that gives the best result in the healing process. Current of different frequency (more than 25 of them) generates the electrotherapy apparatus. More than 200 treatment programs have been developed, which allow us to select for each patient a separate program with individual treatment parameters. One device can be used to treat different diseases or conditions, but the parameters are selected depending on the nature, location and specificity of the lesion. The severity of the process is also taken into account. If the condition is acute, some regimens are used, while those in the chronic condition and rehabilitation are different. Individually selected programs contribute to the high efficiency of treatment. The intensity of pain, fluid,


Electrotherapy has proven itself well in combination with diathermy, especially in the treatment of fasciitis and aponeurositis. The diathermy apparatus module generates high-frequency energy that has the ability to penetrate deeply into tissues and heat them. This increases the activity of biochemical processes in the area, which is exposed, which significantly slows down the processes of degeneration (destruction) of tendons in tendinitis, the formation of scar tissue in fibrosites and aponeurosites, thereby preventing the development of contractures and allows to avoid operations.
The effect of the apparatus is also to prevent the formation of calcines and the reverse development of the latter in the initial stages. This is an important effect in the defeat of the tendon ducts (carpal, guillon, tarsal), since it allows to avoid thickening of the tendons, and accordingly to achieve complete recovery without surgery.