Chronic pain is a serious medical problem that requires long-term adequate therapy and a comprehensive approach. It is the need for long-term adequate therapy that makes it urgent and appropriate to apply measures that reduce the intensity of pain and the duration of treatment . Today, these measures are physiotherapy procedures.





Physiotherapy methods in the treatment of neuropathic pain
Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser, Laser tissues), which is especially important when available hypoxia and inflammation. LT NILV frequency of 200-250 Hz
The mechanism of action of laser radiation on the body is based on the photochemical changes of biomolecules that partially affect the biophysical properties of tissues and the biochemical processes that occur in them. That is, low-intensity laser radiation (NILW) acts at the level of cell membranes, influences the course of redox processes. Under the influence of LP in the body, neuroreflex and neurohumoral reactions occur, sympathoadrenal and immune systems are activated, the concentration of adaptive hormones is increased. Laser radiation improves the tone and elasticity of blood vessels, increases blood levels of brain and peripheral vessels, promotes the regression of various vegetative vascular dysfunctions, improves the speed of the motor impulse along the peripheral nerves. NILV exerts vasodilator, stimulant, analgesic, anti-inflammatory effects, improves metabolism, bioenergy capabilities at the molecular level, resulting in optimized regulatory processes.

Magnetic ultrasound scan (phonophoresis) with NSAIDs - deep penetration of NSAIDs into tissues at the site of inflammation under the influence of ultrasonic vibrations. procedures: 10

Microwave resonance therapy (MRI) or (EMH MMD) - a method of local therapy of electromagnetic waves of the millimeter range of non-thermal intensity (up to 10 mW / cm2) is accompanied by a mild anti-edema, analgesic effect. To date, reliable data have been obtained that, when using MRI or EMH, MMD significantly reduces pain and produces a muscle relaxant effect, improves microcirculation, normalizes blood pressure. At the biochemical level, the normalization of the ratio of neurohumoral substances: serotonin, ACTH, cortisol, endorphins, and enkephalins after the procedure session was proved. The wavelength is 5.6 mm; 7.1 mm Power 3-5mW. Number of procedures 10-15
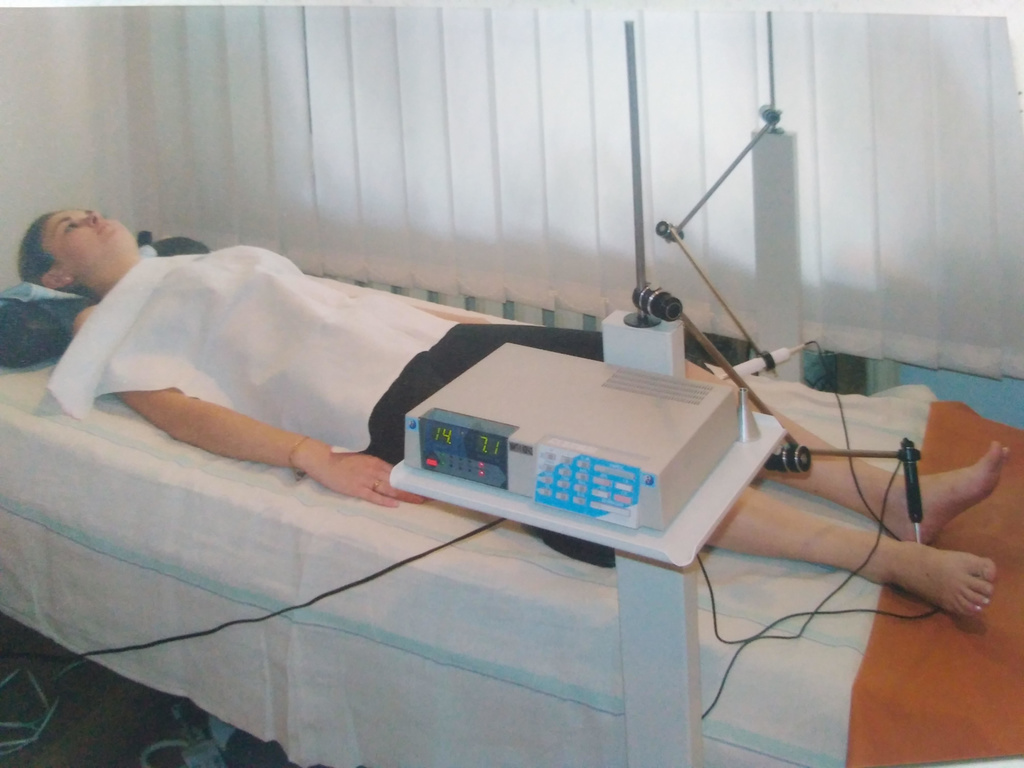
Magnetotherapy-low-frequency magnetic variable field increases the speed of conducting the potential of action on the nerve, increases the excitability of nerve fibers, reduces perineural edema. In addition, low-frequency MP magnetotherapy restores the functional properties of the afferent neurons of pain-sensitive conductors, leading to significant attenuation or termination of impulse from the focus of pain! Magnetotherapy is shown at all stages of neuropathic and mixed. The rationale is pronounced anti-edema, anti-inflammatory action, indirect stimulation of venous outflow, improvement of rheological properties of blood. We apply a frequency of 10Hz. Magnetic Induction Options - Individual Selection! The course of treatment with daily regimen - up to 7 days.

Electrotherapy is used in 2 variants
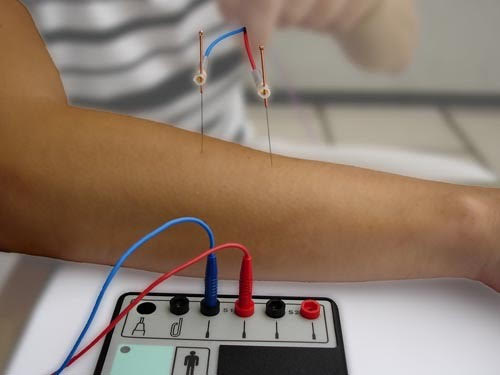
1.Electrotherapy zonal penetration method (influence on reflexogenic zones by weak stimulation at fixed electrodes)
2.Electropuncture (influence on acupuncture points) by direct or alternating current up to 20 mA with frequency from 2-5 Hz to 70-200 Hz.
Changing the pulse rate allows you to achieve a selective effect on different nerve endings: motor, sensory, autonomic. Excitation of sympathetic nerves 15 Hz; parasympathetic 20-100 Hz; vasodilator effect of 20-70 Hz; 80-200 Hz effectively inhibits nociception. However, the most pronounced prolonged effect of inhibition of nociception occurs at a frequency of 5-12 Hz-stimulation of endogenous opiate long-acting system due to the effect on TA
Rehabilitation of patients after neurosurgical removal of intervertebral hernias is an important step. The need for its implementation is based on long-term follow-up of operated patients who went to the clinic for pain in the lumbar or leg, which did not fully or appear after a certain period after surgery, through relapses of the intervertebral hernias, scar formation and joint process. In order to prevent the development of complications, rehabilitation measures have been developed that provide for the implementation of certain recommendations.
- Active postoperative period: gait, light unloading postures and exercises, medication correction according to the individual condition of each patient, in case of muscular weakness in the arm or leg, electrical stimulation, massage.
- Early postoperative rehabilitation is recommended 1.5-2 months after surgery and involves a combination of physiotherapy measures
The approach to each patient is purely individual in nature, it is not always easy to make the decision, but we try to provide high quality advisory assistance to anyone who applies to our "Health Practice".
